Trusted by AML Compliance Leaders Worldwide


Know Your Business - Streamlined KYB Solutions
Accelerate beneficial ownership & UBO discovery to simplify complex ownership structures with corporate onboarding, supporting documents, & questionnaires.
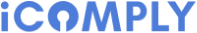
Know Your Customer - Automate KYC Verification
Automate identity verification, liveness, face-match, geolocation, supporting documents, & questionnaires.
Anti-Money Laundering - Global AML Screening
Global AML checks are monitored daily for sanctions screening, politically exposed person screening, and adverse media screening.
Start your free trial of iComply!
Cancel Anytime. No Questions Asked.
Process Failures Cost You More
Time & Money Every Year
Disjointed Vendors
Fragments your operations, consumes copious development resources, and invites risk to slip through the cracks.
Manual Processes
Restrains your businesses growth, demands excessive human capital, and cause significant human error.
Negative Customer Experiences
Reduces your public trust, brand value, and competitive advantage.
Streamline Your KYB, KYC, & AML Compliance
Eliminate Vendor Complexity
Onboarding to ongoing, we help you manage the complete lifecycle of a natural person or legal entity.
Boost Efficiency & Effectiveness by up to 90%
Configure intuitive workflows and automation to apply your policies and procedures at scale.
Improve Customer Satisfaction by over 25%
Reduce friction with a variety of options for quick and convenient single touchpoints.

World-Class Privacy, Security, & Encryption
Adhere to data protection regulations including SOC2 and ISO 27001, CCPA, GDPR, PPIA, PIPEDA, PCI, and more.
Process and secure all sensitive data, documents, and biometrics on the user’s own device, not our servers, using the power of edge computing.
Leverage best practices with end-to-end encryption (TLS1.2, SSL, AES256) to store member data on your servers or clouds.
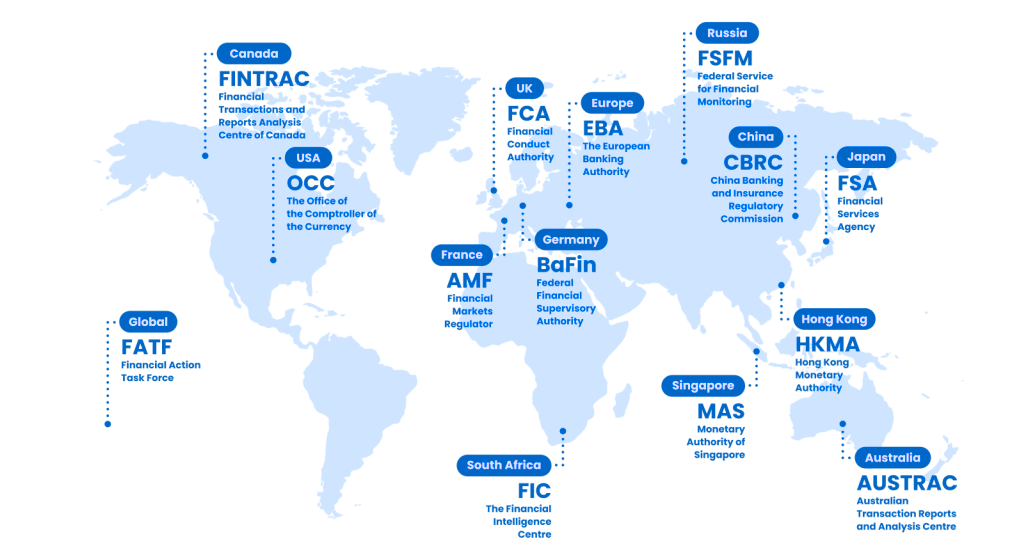
Global AML Compliance
Streamline and automate compliance in 195 countries.
14,000+ Identity Verification Documents
3,000+ Watchlists for Sanctions Screening
11,000+ Trusted Sources for Adverse Media Checks
PEPs Class 1-4: Politically Exposed Persons
We have settled in with your service and are very impressed. I have every confidence in iComply for the UK, where increasing pressure from regulators to not only improve AML compliance, but also to be able to demonstrate it.
Frequently Asked Questions
Learn more about about AML compliance, customer due diliegnce, and how iComply can support your business
Start your free trial of iComply!
Cancel Anytime. No Questions Asked.